Candida auris (C. auris) is an emerging fungal pathogen that has recently risen to public notoriety as an increasing cause of hospital-acquired, or nosocomial, infections. The fungus can cause severe infections that are difficult to treat. Furthermore, it has been linked to outbreaks in hospitals and long-term-care facilities around the world.
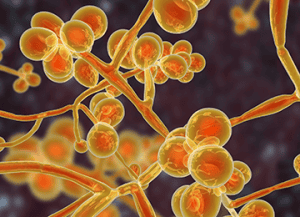
The Candida Auris organism was first officially identified in Japan in 2009 but has since been isolated from yeast culture collections from 1996 in South Korea. Although C. auris has been present in hospital environments for nearly 20 years, the growing concern revolves around the rapid evolution of microbial resistances to echinocandins, the primary antifungal used to treat invasive yeast infections, as well as to other antifungals. These growing resistances lead to difficulties in treatment options for the infections and have a resulted in a call for health care product manufacturers to increase research in areas such as effective contamination control.
An additional challenge with C. auris is that it can survive on surfaces in health care facilities for long periods of time. This means that even if a patient has been successfully treated for a C. auris infection, the fungus could still be present on surfaces, with the potential to infect other patients. To prevent and control outbreaks of C. auris in health care settings, it is important to follow proper protocols for infection prevention and control. This includes thorough cleaning and disinfection of surfaces and equipment, using appropriate personal protective equipment (PPE), and isolating patients who are infected with the fungus.

This pathogen’s longevity on surfaces offers an interesting contrast to the most recent COVID-19 pandemic. The pandemic prompted an aggressive industry response to demonstrate virucidal efficacy on surfaces in many product categories. In fact, regulatory agencies, such as the US Environmental Protection Agency (EPA), offered new and expedited label-claim pathways, e.g., List N and residual surface efficacy, as a result of public and industry pressures. While COVID-19 is predominantly viewed as respiratory virus, mitigation of surface transmission certainly played a large role in our cumulative infection prevention plan. While no specific regulatory actions like this have been issued against C. auris, there is certainly awareness and discussion in the industry about antifungal efficacy against this pathogen.
As our health care system continues to ramp up its response to increased infection rates linked to C. auris, we should reflect on the similarities of previous pathogens that emerged. The COVID-19 pandemic changed the way the public understands health care and safety. The full effect of this paradigm shift has yet to be realized, but we can be certain antimicrobial efficacy will be a main consideration of our cohesive public health and industry response.
Antimicrobial Efficacy Testing at Nelson Labs
At Nelson Labs Bozeman we host panels of C. auris from the Centers for Disease Control and Prevention (CDC) and Food and Drug Administration (FDA) Antimicrobial Resistance (AR) Isolate Bank. These isolates range from being minimally resistant to antifungals to resistant to multiple antifungals. Our team also offers the expertise to meet specific regulatory requirements, e.g., EPA hard-surface disinfectant registration, as well as to develop custom studies to meet your specific data criteria. We offer the following efficacy testing options within the consumer and health care industries:
- Disinfectant registration and testing (fungicidal, antibacterial, virucidal, and resistant strains)
- Antimicrobial surface treatment testing
- Antimicrobial fabrics and treatments
- Residual efficacy testing for surfaces and disinfectants
- Antimicrobial suspension and time kill test
- MIC/MBC – antimicrobial efficacy
- Antimicrobial preservative efficacy evaluations
- Facility cleaning and procedure validation
If you have any questions, please reach out to our team at [email protected]. We are ready to help you.


